Introduction
Menopause is often spoken about in terms of hot flushes, mood swings, and restless nights. But for many women, there’s another symptom that creeps in quietly and leaves you second-guessing your footing – dizziness. It might happen when you stand up too quickly, mid-way through a meeting, or while browsing the supermarket aisles. At first, you brush it off. But when it keeps returning, you start to wonder if something’s wrong.
These moments aren’t just inconvenient. They can make everyday tasks feel unpredictable – the quick dash for a train, climbing stairs in heels, even enjoying a glass of wine with friends. And because dizziness is often invisible to others, it’s easy to feel alone with it, quietly trying to steady yourself without drawing attention.
Here’s the truth: dizziness during menopause is common, and it has clear, manageable causes. Sometimes it’s hormonal. Sometimes it’s lifestyle-related. Occasionally, it’s a sign of something that needs medical attention. This article will help you understand the different types of dizziness, what’s triggering yours, and the practical steps – from hydration tweaks to targeted therapies – that can help you feel steady on your feet again.
Before we get into solutions, let’s start with exactly what dizziness and light-headedness mean during menopause – and how to tell them apart.
Understanding Dizziness and Light-Headedness in Menopause
Feeling suddenly unsteady on your feet can be unnerving – especially if it strikes without warning. During menopause, dizziness and light-headedness are more common than many realise, often linked to the hormonal shifts that affect multiple systems in the body. Understanding what is happening is the first step towards feeling more in control.
Knowing the difference: dizziness, light-headedness, and vertigo
-
Dizziness is a general sense of being unsteady or off-balance, almost as if the world is moving under your feet.
-
Light-headedness feels more like you might faint – a floating, disconnected sensation in your head.
-
Vertigo is a spinning or tilting feeling, as though the room is rotating.
Many patients find it hard to pinpoint which one they have, especially if episodes are brief. If it feels sudden and intense, note the details for your GP.
Common balance disturbances linked to menopause
-
Vestibular changes – Fluctuating hormones can affect the inner ear, which plays a key role in balance.
-
Postural hypotension – A drop in blood pressure when standing up quickly, leading to light-headedness.
-
Benign paroxysmal positional vertigo (BPPV) – Brief spinning sensations triggered by certain head movements.
Episodes may last seconds or minutes, but the after-effect – that odd sense of needing to steady yourself against the wall – can linger longer.
Closing your eyes and taking a deep breath might help in the moment, but knowing the possible causes makes it easier to plan your next step. If dizziness is persistent, worsening, or accompanied by other symptoms, it’s important to speak to a healthcare professional for a full assessment.
The Hormonal Connection
Hormonal fluctuations during peri-menopause and menopause can influence almost every part of the body – including systems you might not expect, like balance and spatial awareness. Many women are surprised to discover that the same shifts driving hot flushes or mood changes can also trigger dizzy spells.
How oestrogen and progesterone support balance
- Oestrogen’s role – This hormone helps maintain healthy blood vessels in the brain and supports neurotransmitters that regulate balance signals. When levels drop, blood flow and nerve signalling can be disrupted.
- Progesterone’s role – Known for its calming effect on the nervous system, progesterone can influence how your body processes sensory input from the eyes, ears, and joints.
Reduced levels of both can make the vestibular system (your body’s balance control centre) more sensitive to changes.
The ripple effect on other systems
- Circulatory system – Lower oestrogen can contribute to changes in blood pressure regulation, leading to momentary drops when you stand up too quickly.
- Blood sugar control – Hormonal shifts can make blood sugar fluctuations more pronounced, especially if meals are irregular.
- Temperature regulation – Hot flushes can trigger rapid changes in blood vessel dilation, sometimes leading to dizziness mid-episode.
It’s a bit like adjusting to a dimmer switch that keeps changing brightness – your body is constantly recalibrating.
Recognising the hormonal link isn’t just about reassurance – it also points towards potential solutions, from dietary adjustments to medical interventions like hormone replacement therapy (HRT), which some women find stabilises their symptoms.
Other Contributing Factors Beyond Hormones
While hormonal shifts are a key driver of dizziness during menopause, they are rarely the whole story. Everyday habits, environmental factors, and underlying health conditions can all tip the balance – literally. Identifying these triggers can be as crucial as addressing hormonal changes.
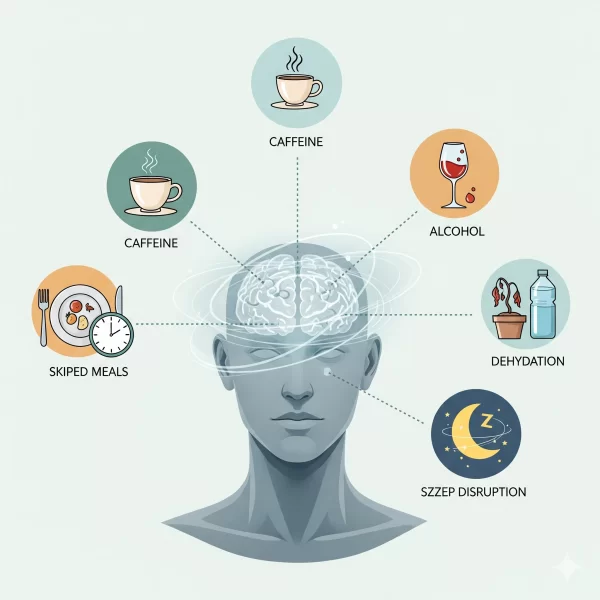
Lifestyle triggers you might overlook
- Caffeine and alcohol – Both can affect hydration and blood vessel dilation, making dizziness more likely.
- Skipped meals – Low blood sugar can cause light-headedness, especially during busy workdays when lunch is an afterthought.
- Dehydration – Even mild dehydration can reduce blood volume, affecting brain oxygen levels.
- Sleep disruption – Poor sleep, whether from night sweats or stress, impacts your body’s ability to regulate balance.
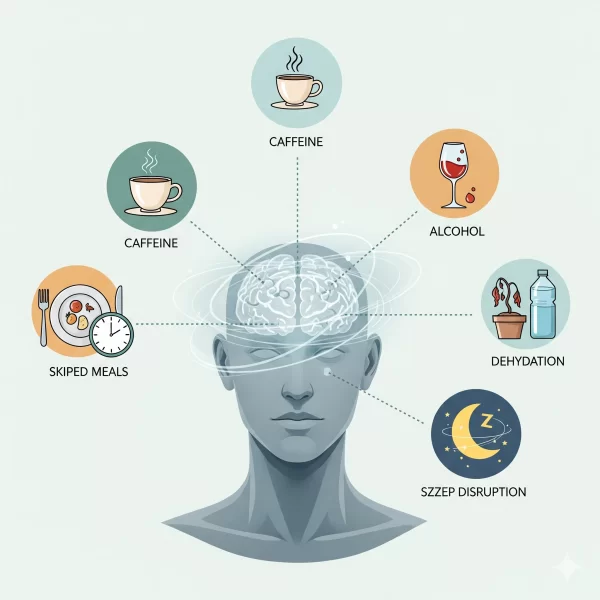
Keeping a simple “dizziness diary” – jotting down what you ate, drank, and did before each episode – can reveal surprising patterns.
When underlying health conditions play a part
- Anaemia – Low iron reduces oxygen delivery to the brain.
- Thyroid disorders – Both underactive and overactive thyroids can influence metabolism and balance.
- Cardiovascular issues – Heart rhythm changes or narrowing of blood vessels can cause sudden drops in brain oxygen.
- Inner ear disorders – Not all dizziness is menopause-related; conditions like Ménière’s disease can overlap.
Seek medical advice promptly if dizziness is accompanied by sudden hearing loss, severe headache, or weakness.
By spotting these contributing factors early, you can work with your GP or specialist to address them directly, often reducing symptoms significantly.
Recognising When to Seek Help
Most menopause-related dizziness is mild and short-lived, but there are moments when it signals something more serious. Knowing the difference can help you act quickly and confidently if needed.
Red flag symptoms that need urgent attention
- Sudden, severe headache – Especially if unlike any you have had before.
- Chest pain or pressure – Could signal a heart issue requiring immediate care.
- Slurred speech or facial drooping – Possible signs of a stroke.
- One-sided weakness or numbness – Another potential stroke symptom.
- Sudden hearing loss – Could indicate an inner ear emergency.
If any of these occur, call 999 or seek emergency medical attention right away.
How professionals diagnose dizziness
- Medical history review – Your GP will ask about the nature, timing, and triggers of your episodes.
- Physical examination – Includes blood pressure checks, balance assessments, and neurological tests.
- Blood tests – Can reveal anaemia, thyroid issues, or blood sugar imbalances.
- Specialist referrals – ENT specialists, neurologists, or cardiologists may be involved if the cause isn’t clear.
A flowchart or symptom timeline can be helpful to bring along, helping clinicians spot patterns you might not notice day-to-day.
Being clear on when to seek help not only protects your health but also brings peace of mind. The next step is to explore practical ways to reduce dizziness and regain your sense of steadiness.
Practical Strategies for Relief
Managing dizziness during menopause often means a mix of lifestyle adjustments and, where appropriate, targeted medical care. The aim is not just to reduce episodes but also to feel more confident going about daily life without that lingering fear of the next dizzy spell.
Every day adjustments you can start today
- Stay hydrated – Aim for steady water intake throughout the day rather than gulping large amounts at once.
- Move mindfully – Stand up slowly from sitting or lying positions to avoid sudden blood pressure drops.
- Eat balanced meals – Include protein, healthy fats, and complex carbohydrates to maintain stable blood sugar.
- Breathe deeply during symptoms – Slow, steady breathing can help your nervous system reset.
- Limit alcohol and caffeine – Both can affect balance and hydration.
Medical and complementary treatment options
- Hormone replacement therapy (HRT) – May help stabilise hormonal fluctuations that affect balance.
- Vestibular rehabilitation – A type of physiotherapy that retrains your balance system.
- Acupuncture – Some women report reduced dizziness frequency with regular sessions.
- Medication review – Your GP can check if current prescriptions are contributing to dizziness.
Always discuss treatment options with a qualified healthcare professional to tailor an approach that fits your health history and needs.
By combining daily habits with professional guidance, many women find their symptoms become less disruptive – and sometimes disappear entirely.
Living Well Despite the Wobbles
Even when dizziness is under control, the memory of past episodes can linger. Some women describe walking into a crowded supermarket and feeling a wave of nerves, not because they feel dizzy in the moment, but because they remember how it felt last time. The goal here is to rebuild confidence while keeping self-care at the forefront.
Protecting your emotional well-being
- Acknowledge the anxiety link – Dizziness can trigger worry, which in turn can make symptoms worse.
- Gradual exposure – Reintroduce activities that previously triggered dizziness in small, manageable steps.
- Mind-body practices – Yoga, tai chi, or gentle Pilates can improve both balance and mental calm.
- Stay socially connected – Isolation can amplify anxiety; trusted friends or support groups can make a difference.
Finding the right support network
- NHS menopause clinics – Offer access to specialist advice and treatment plans.
- Private practitioners – Can provide tailored therapies and more flexible appointment times.
- Online communities – Forums and groups where women share tips, reassurance, and success stories.
- Local classes – Balance-focused exercise classes can be both social and therapeutic.
Living well with occasional dizziness means knowing your body’s signals, making smart adjustments, and having strategies to fall back on. Over time, the focus shifts from “Will this happen again?” to “I know what to do if it does.”
Conclusion
Menopause can change the rhythm of your days in ways you might not expect, and dizziness is one of those subtle yet disruptive shifts that deserves more attention. Understanding the interplay of hormones, lifestyle factors, and underlying health conditions is not just about symptom management – it’s about reclaiming a sense of steadiness, both physically and emotionally.
What matters most is recognising that you’re not alone, and that with the right strategies, these moments of imbalance can become less frequent and far less daunting. From small, consistent daily habits to professional interventions, there are clear, evidence-based steps you can take to regain confidence in your body’s balance.
If dizziness has been affecting your daily life, consider speaking with a qualified menopause specialist or trusted GP to explore your options. And if you’re ready to go deeper, our related guides on hormonal health and midlife wellness offer practical, expert-led insights to help you feel informed and supported. Your next steady step starts with knowing what’s possible.